Biostimulation Effects and Temperature Variation in Stimulated Dielectric Substance (Diabetic Blood Comparable to Non-Diabetic Blood) Based on the Specific Absorption Rate (SAR) in Laser Therapy
Keywords:
Dielectric properties, specific absorption rates, diabetic blood, low-level laser therapy, impedance, diabetic blood.Abstract
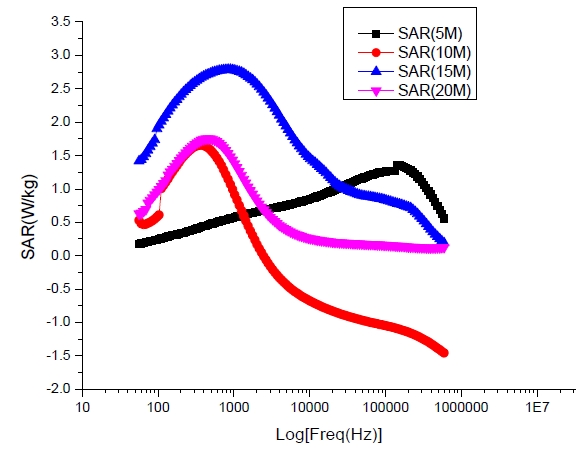
Human blood exposed to irradiation absorbs electromagnetic energy which consequently effect temperature variation. The evaluation of Specific Absorption Rate (SAR) of human blood helps to ascertain the values for optimum laser power, time, and temperature variation for fair therapy to avoid blood-irradiation pollution but to enhance its rheological properties when using lasers. Prior knowledge of blood SAR evaluating its dielectric properties is significant, but this is under investigation. We investigate the appropriate SAR threshold value as affected by temperature variation using fundamental blood dielectric parameters to optimize the effect of low-level laser therapy based on physiological and morphological changes of the stimulated diabetic blood. Studies were carried out with Agilent 4294A impedance analyser at frequencies (40Hz – 30 MHz) and designed cells (cuvettes) comprises of electrodes were used in the pre- and post-irradiations measurements. At different laser power outputs, blood samples were subjected to various irradiation durations using portable laser diode-pumped solid state of wavelength 532 nm. Results showed laser at low energy is capable of moderating morphologically the proportion of abnormal diabetic red blood cells. Hence, there is a significant effect using a laser at low energy, as non-medicinal therapy in controlling diabetic health conditions. The positive biostimulation effects on the irradiated diabetic blood occurred within absorbance threshold SAR values range of 0.140?0.695 W/kg and average temperatures range of 24.2?28.0 0C before blood saturation absorbance peak. There is morphological stimulation at a laser power of 50 mW for an exposure time of 10–15 minutes and 60 mW for 5–10 minutes of laser therapy that demonstrates better blood rejuvenated conditions. This occurred within the threshold SAR of 0.140?0.695 W/kg and average temperatures range of 24.2?28.0 0C. Therefore, the diabetic blood irradiated using laser output powers of 70 and 80 mW during exposure durations of 5,10, 15 and 20 minutes rather bio-inhibits positive blood stimulation which has resulted to crenation due to excessive irradiation.
Published
How to Cite
Issue
Section
Copyright (c) 2021 Journal of the Nigerian Society of Physical Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.
How to Cite
Most read articles by the same author(s)
- Terver Daniel, F. Eriba-Idoko, J. O. Tsor, S. T. Kungur, E. O. Enokela, F. Gbaorun, E. C. Hemba, A. A. McAsule, N. S. Akiiga, P. O. Ushie, Effects of Repeated Frying on Physical Properties of Cooking Oil obtained from Local Markets in Makurdi Metropolis, Benue State, Nigeria. , Journal of the Nigerian Society of Physical Sciences: Volume 3, Issue 4, November 2021