Dynamical and optimal control analysis of lymphatic filariasis and buruli ulcer co-infection
Keywords:
Neglected tropical disease, Mathematical model, Lymphatic filariasis, Buruli ulcer, Optimal controlAbstract
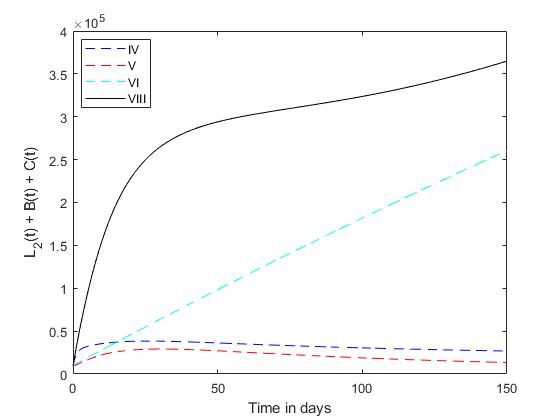
This study delves into the dynamics of lymphatic filariasis and buruli ulcer coinfection, two overlooked yet impactful tropical diseases. With lymphatic filariasis, commonly referred to as elephantiasis, and buruli ulcer, a chronic affliction caused by mycobacterium ulcerans, both posing significant health challenges, understanding their interaction is crucial. Utilizing a mathematical model, this research aims to analyze the dynamics of this coinfection, elucidating its complexities. The study establishes the local asymptotic stability of the disease-free equilibrium and calculates the basic reproduction number using the next generation matrix. It uncovers transcritical and backward bifurcation phenomena within the model. Additionally, the integration of time-dependent controls enables the exploration of optimal disease management strategies. Numerical simulations highlight the efficacy of employing a comprehensive approach, utilizing all available controls simultaneously, as the most effective strategy for disease control. These findings underscore the importance of integrated interventions in combating lymphatic filariasis and buruli ulcer coinfection, offering valuable insights for public health policymakers and practitioners.
Published
How to Cite
Issue
Section
Copyright (c) 2024 Helen Olaronke Edogbanya, Emmanuel Sabastine, Rosalio G. Artes Jr., Regimar A. Rasid

This work is licensed under a Creative Commons Attribution 4.0 International License.